WHO Warning: Mpox cases are climbing rapidly with a much higher death rate
Update — August 14, 2024, 12:44 PM ET
The World Health Organization (WHO) has just labeled the mpox outbreaks in Congo and various parts of Africa as a global emergency.
The virus is on the rise, with cases popping up in both kids and adults across more than a dozen countries. Unfortunately, Africa is facing a serious vaccine shortage.
Earlier this week, the Africa Centers for Disease Control and Prevention (Africa CDC) declared it a public health emergency. With over 500 reported deaths, they’re urgently asking for international help to curb the virus’s spread.
“This should concern us all… The potential for further spread within Africa and beyond is very worrying,” said WHO Director-General Tedros Adhanom Ghebreyesus.
Mpox surging in over a dozen countries
According to the Africa CDC, mpox, or monkeypox, has been detected in 13 countries this year, with Congo accounting for more than 96% of all cases and fatalities.
In fact, cases have surged by 160% and deaths by 19% compared to last year. So far, there have been over 14,000 reported cases, leading to 524 deaths.
“We’re now at a point where mpox poses a risk to many more neighboring countries in and around central Africa,” said Salim Abdool Karim, a South African infectious diseases expert leading the Africa CDC emergency group. He pointed out that the new strain of mpox coming from Congo has a death rate of about 3-4%.
Back in 2022, the WHO declared mpox a global emergency after it spread to over 70 countries that hadn’t seen any cases before. That outbreak largely affected gay and bisexual men, with less than 1% of cases resulting in death.
Michael Marks, a professor of medicine at the London School of Hygiene and Tropical Medicine (LSHTM), supports the emergency declaration. “It’s a failure of the global community that things had to escalate to this extent to mobilize the necessary resources,” he said.
This situation raises important questions about global health preparedness and how interconnected our societies are. As we work to tackle these challenges, understanding the implications of mpox and promoting international cooperation is crucial.
Public vigilance declines
It’s easy to forget about public threats that are no longer in the headlines, but when it comes to health, forgetting can be a deadly trap. Take mpox – a disease that’s been shuffling in and out of the world’s spotlight for years.
Today, two years after the World Health Organization (WHO) triggered a global health alarm over an mpox outbreak, this notorious enemy has reemerged, this time spreading its lethal tendrils across African nations.
But as the stakes rise, public memory and understanding about this disease seem to have taken a nosedive.
Public perceptions about mpox
The evidence for this public “out of sight, out of mind” mentality comes from none other than the respected Annenberg Public Policy Center of the University of Pennsylvania.
Under the leadership of Kathleen Hall Jamieson, the center has been closely monitoring public knowledge and perceptions about mpox.
Here’s the truth: as media attention shifted, the threat of mpox didn’t just pack up and leave. Instead, it quietly snuck into the shadows, covertly marching across the globe as a hidden potential health crisis.
“The speed with which the public learned needed information about mpox in the summer of 2022 was a tribute to effective communication by the public health community,” said Jamieson.
“That same expertise should now be deployed to ensure that those at risk remember mpox’s symptoms, modes of transmission, and the protective power of vaccination.”
Diving into the data
The center’s ASAPH survey conducted in July 2024 sheds light on some hard truths. For starters, only five percent of Americans are worried about contracting mpox in the next three months — a huge drop from 21 percent back in August 2022. A mere nine percent are concerned about their families being hit by the disease.
The public’s understanding that mpox is less contagious than Covid-19 has plummeted from 41 to 17 percent.
Knowledge that men who have sex with men are at a higher risk of infection has spiraled down from 63 to 34 percent. Furthermore, recognition of the existence of an mpox vaccine has fallen from 61 to 45 percent.
Unmasking mpox
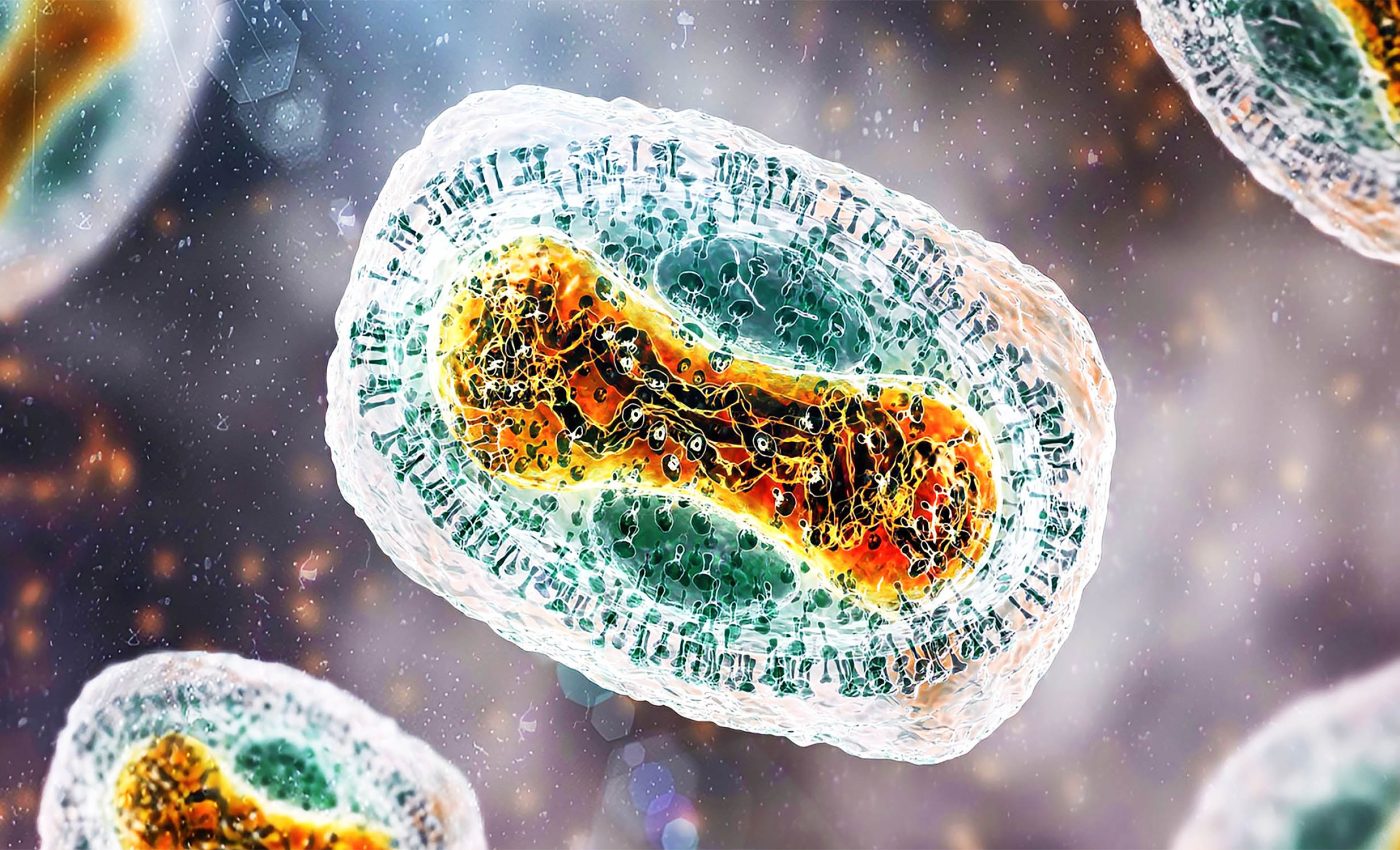
Understanding a disease is often the first armor in our battle against it. Mpox, first identified in 1958, is a rare but deadly member of the orthopox virus family. It brings with it a medley of symptoms — fever, chills, headaches, muscle aches, swollen lymph nodes, and painful rashes.
The transmission of the disease is through contact with infected animals or close interaction with an infected person, including sexual contact and touching with contaminated materials.
Today’s outbreak features a different face of mpox — clade I. This strain is particularly relentless in its attack on infants and children under the age of 5.
A report from the WHO reveals this led to the unfortunate loss of 511 lives, with 62 percent of the deaths involving children under the age of 5 in the Democratic Republic of Congo.
While clade I currently resides within the boundaries of central and east Africa, clade II, seen in the 2022 outbreak in the U.S., is still lurking around.
The majority of these cases are found in individuals who didn’t receive the vaccine or got only one of the two doses necessary.
Vigilant public awareness on mpox
In the face of resurfacing threats like mpox, fostering awareness and understanding among the public is not merely advisable; it is essential.
Public education campaigns must proactively combat misinformation and rekindle interest in health implications linked to mpox.
This strategy should focus on providing clear, accessible information about transmission, symptoms, and the importance of vaccination.
Engaging a diverse audience through trusted community leaders and health professionals can amplify the message, ensuring that individuals at higher risk understand the necessity of preventive measures.
Furthermore, maintaining the momentum of the discussion around mpox – even when it fades from mainstream media – can help keep the public informed and alert, ultimately contributing to better health outcomes and preparedness.
The lessons learned from past outbreaks underscore the critical need for a well-informed populace that is prepared to respond to health threats as they present themselves.
Inoculation: Our best bet
Hope, however, is on the horizon. The intention of people to get vaccinated against the disease still holds strong.
The CDC recommends the use of Jynneos, administered in two doses, four weeks apart, for those exposed to the mpox virus and those with risk factors, including men who have sex with men.
Time to kick out complacency and reignite our efforts. Let’s dust off the cobwebs of forgetfulness and strengthen our understanding about mpox. In the face of a pandemic, knowledge is indeed our most powerful weapon.
The Annenberg Public Policy Center continues its tireless efforts to illuminate the public and policy makers about significant health issues.
Their work is a beacon in the darkness, reminding us to remember, relearn, and react to keep the threat of mpox at bay.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—-
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—-













