Alzheimer's may not be a brain disorder, important data was fabricated
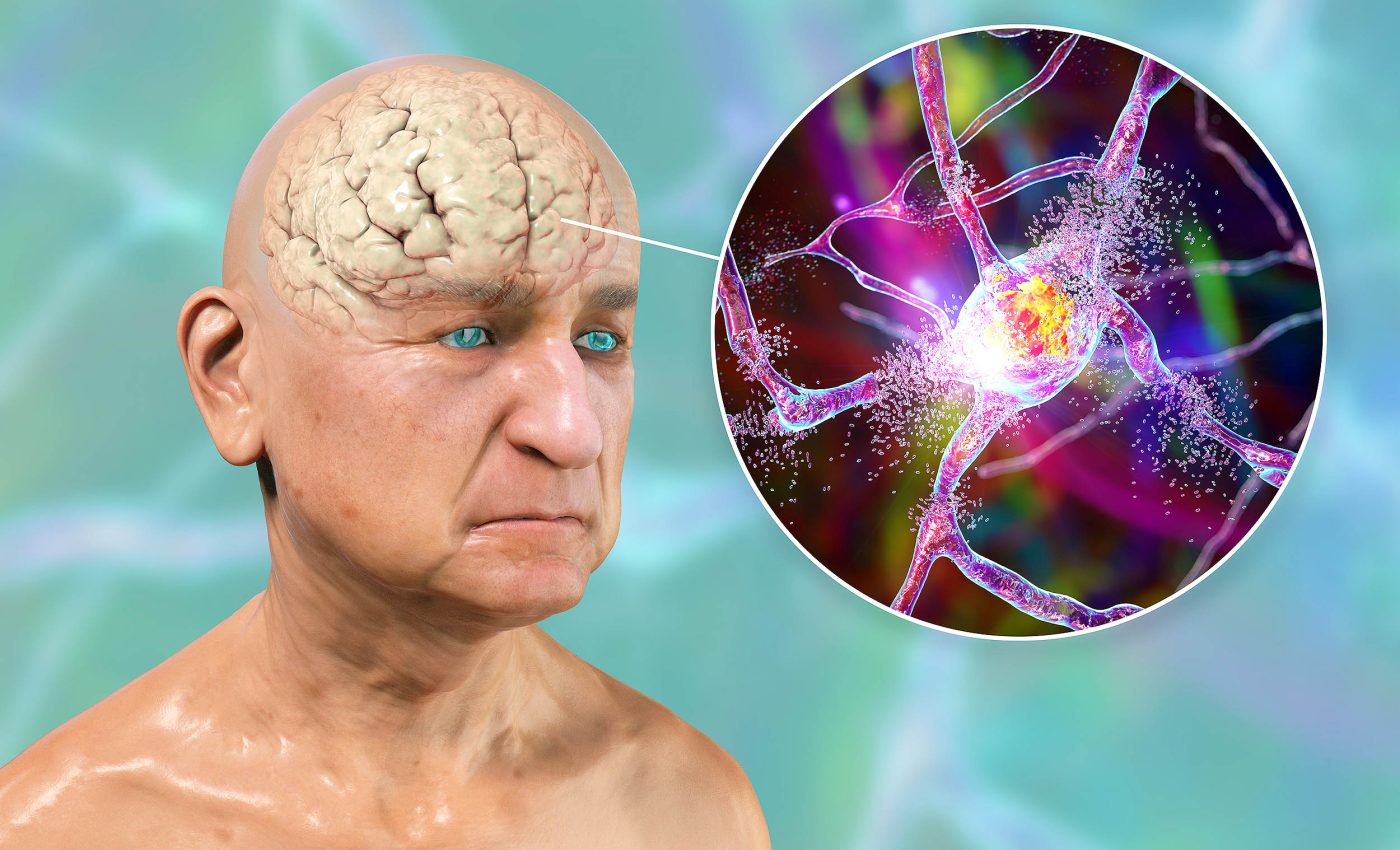
What if everything we thought we knew about a condition was turned on its head? Imagine Alzheimer’s, the notorious affliction of the mind, not being a brain ailment after all, but an autoimmune disorder.
Dr. Donald Weaver, with his team at the Krembil Brain Institute, Toronto, has a radical new theory that presents this exact proposition.
Doubts about Alzheimer’s and the brain
The ongoing pursuit of an Alzheimer’s cure is a journey fraught with controversies and conflicts. A recent revelation in Science magazine stated that the 2006 research paper identifying the beta-amyloid brain protein as the Alzheimer’s cause might have been built on erroneous data.
Around the same time, the U.S. Food and Drug Administration (FDA) approved a drug, aducanumab, meant to target beta-amyloid — an approval mired in controversy due to incomplete and conflicting data.
This approval resulted in an unsettling divide among physicians, with some supporting its chance, and others convinced it should never have seen the light of day.
Dilemma of beta-amyloid
The pervasive concentration, over the years, on beta-amyloid as the main culprit, appears to have led us through a proverbial rabbit hole.
Regrettably, this unwavering focus has not borne fruit in the form of a working drug or therapy.
Dr. Weaver’s lab now redirects the spotlight onto the immune system within the brain, presenting Alzheimer’s as not just a brain disease, but an autoimmune disorder.
Immune system gone rogue
Like any part of our bodies, our brain has an immune system that kicks into action when required – mending wounds, fighting bacterial invasions, and helping repair after trauma.
Dr. Weaver’s team suggests the infamous beta-amyloid might not be an abnormal protein after all, but a normal compound that forms part of the brain’s immune system.
Trouble brews when beta-amyloid’s inability to differentiate between invading bacteria and brain cells causes it to attack and destroy the very cells it should protect, eventually leading to a loss of brain function and, finally, dementia.
Curing Alzheimer’s outside the brain
Promisingly, this new perspective on Alzheimer’s opens up the exploration of alternative immune-regulating pathways, paving the way for potential new treatments.
Conventional drugs used for autoimmune diseases may not work, but don’t lose heart. The answer might lie in tackling other immune-modulating pathways in the brain, providing hope for new and effective treatments.
This is not the only new theory cropping up around Alzheimer’s. Some scientists speculate that Alzheimer’s is a disease of mitochondria, while others argue that it might stem from an infection, particularly by mouth bacteria.
Other scientists are looking into abnormal handling of metals like zinc, copper, or iron in the brain.
Alzheimer’s disease is a global issue
Alzheimer’s, affecting over 50 million people across the globe, with a new diagnosis every three seconds, is a growing public health crisis.
People with Alzheimer’s sometimes fail to recognize their own children or lifelong partners, underscoring the devastating impact of this formidable disease.
As researchers investigate these diverse avenues, collaboration across disciplines becomes imperative.
The challenges of Alzheimer’s demand a consolidated effort from neurologists, immunologists, and pharmacologists, fostering interdisciplinary dialogue to unravel this complex condition.
The urgency to comprehend the multifaceted nature of Alzheimer’s cannot be overstated, for every insight brings us one step closer to not only understanding but potentially eradicating a disease that diminishes quality of life for millions.
Future of Alzheimer’s and brain research
In a refreshing new avenue of research, Dr. Douglas Kelley from the University of Rochester and his team have found an intriguing link between a type of drug used to induce labor in pregnant women and Alzheimer’s.
They found that these drugs could potentially speed up the brain’s waste clearing system, which is dysfunctional in those suffering from Alzheimer’s.
By applying these drugs, which cause muscle contractions, they found some restorative effects. “One can see how this approach, perhaps combined with other interventions, could be the basis for future therapies for these diseases,” Dr. Kelley said.
Whether the answer lies in shifting our view of Alzheimer’s from a brain disorder to an autoimmune disease or in using existing drugs in new ways, the journey to find a solution continues with inexhaustible determination. Through persistent research, the world still hopes for light at the end of the Alzheimer’s tunnel.
—–
Like what you read? Subscribe to our newsletter for engaging articles, exclusive content, and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–













